Redefining Neurovascular Care
Solving Complex Pediatric Diagnoses—Together.
BLT brings together top pediatric specialists from Boston, London, and Toronto to improve outcomes for children with rare cerebrovascular conditions. Our model unites surgical precision, advanced imaging, and real-time case consultation—so no child faces a complex diagnosis without global expertise.
Diseases We’re Fighting Together
BLT is a cross-continental alliance accelerating the pace of discovery in rare disease diagnosis and treatment. By combining clinical expertise, data-sharing, and cutting- edge research, we’re redefining what’s possible. Check out some of the rare diseases we specialize in below.
Cerebral Proliferative Angiopathy (CPA)
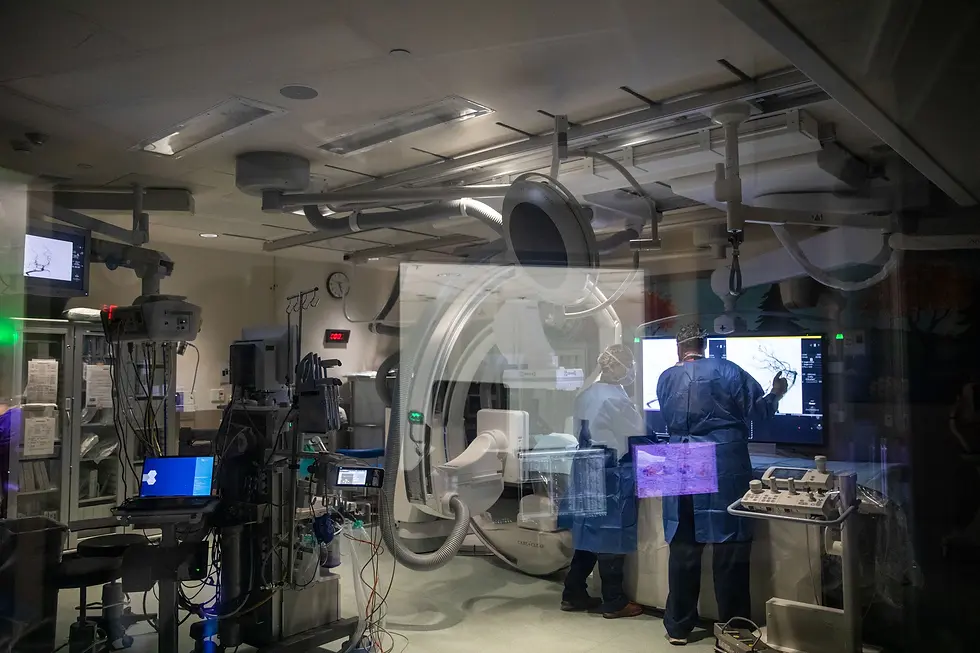
Cerebral Proliferative Angiopathy is a rare vascular malformation involving a dense web of small, abnormal blood vessels mixed with healthy brain tissue. Unlike discrete AVMs, CPA tends to cover a wide area, making surgical removal risky. The slow growth and diffuse nature of the vessels can cause chronic symptoms such as headaches, seizures, cognitive difficulties, and progressive neurological deficits, often over years. Diagnosis typically involves advanced imaging techniques like MRI or angiography. Treatment is highly individualized, ranging from careful observation to targeted endovascular therapy, depending on the patient’s symptoms and the lesion’s location.
Moyamoya Disease
Moyamoya disease is a progressive condition where the main arteries supplying blood to the brain—particularly the internal carotid arteries—become narrowed or blocked over time. In response, the brain forms a delicate network of tiny collateral vessels to maintain blood flow, but these vessels are fragile and prone to bleeding or clotting. Symptoms can include recurrent strokes or transient ischemic attacks, often starting in childhood, as well as cognitive decline or seizures in later stages. Surgical revascularization procedures, such as direct or indirect bypass surgery, are often recommended to improve blood flow and reduce the risk of further strokes.
Moyamoya Disease | Boston Childrens Hospital
Moyamoya Day: Shedding Light on a Rare Paediatric Condition | International and Private Care - GOSH

Vein of Galen Malformation (VOGM)
A Vein of Galen Malformation is a serious, high-flow vascular anomaly that develops during fetal brain development. In this condition, abnormal connections form between arteries and the vein of Galen, bypassing normal capillary networks. This can result in significant blood flow directly into the vein, placing enormous strain on the heart and potentially leading to heart failure, hydrocephalus, or developmental delays in infants. Early detection, often via prenatal ultrasound or neonatal imaging, is crucial. Modern endovascular embolization techniques—sometimes performed in multiple stages—have dramatically improved survival rates and long-term outcomes.
Brain Aneurysm
A brain aneurysm occurs when a weakened section of a brain artery wall bulges outward, creating a balloon-like sac. While many aneurysms remain stable and symptom-free, some can leak or rupture, causing a subarachnoid hemorrhage—a potentially fatal form of stroke. Warning signs of an unruptured aneurysm may include localized headaches, vision changes, or nerve compression, but rupture often occurs without warning, presenting as a sudden, severe “thunderclap” headache. Risk factors include hypertension, smoking, and certain hereditary conditions. Treatment options, such as surgical clipping or endovascular coiling, aim to secure the aneurysm and prevent rupture.


Cavernous Malformations
Cavernous malformations, also known as cavernomas or cerebral cavernous malformations (CCMs), are clusters of abnormal, thin-walled blood vessels in the brain or spinal cord that resemble small “mulberry-like” structures. These lesions can leak blood slowly over time or sometimes bleed more significantly, leading to symptoms such as headaches, seizures, neurological deficits, or stroke-like events. While some cavernous malformations remain silent and are discovered incidentally on imaging, others require careful monitoring or surgical intervention depending on their size, location, and risk of bleeding. Ongoing research is focused on better understanding the genetic causes, natural history, and optimal management strategies to improve outcomes for patients living with this condition.
Arteriovenous Malformations (AVMs)
Arteriovenous malformations (AVMs) are rare, abnormal tangles of blood vessels in which arteries connect directly to veins without the usual network of tiny capillaries between them. This creates high-pressure blood flow that can weaken vessel walls and increase the risk of bleeding into the brain. AVMs may cause headaches, seizures, or neurological symptoms depending on their size and location, though some remain asymptomatic until a rupture occurs. Treatment options—such as surgery, radiosurgery, or embolization—are carefully considered based on individual risk, while ongoing research is deepening our understanding of their development and best management strategies.

Arteriovenous Fistulas (AVFs)
Arteriovenous fistulas (AVFs) are abnormal, direct connections between an artery and a vein that bypass the normal capillary system. In the brain or spinal cord, this high-flow connection can place strain on surrounding blood vessels, leading to symptoms such as headaches, seizures, pulsatile tinnitus, or even bleeding. AVFs may be congenital or acquired following trauma, surgery, or blood clots. Diagnosis typically relies on advanced imaging, and treatment—ranging from endovascular embolization to surgery—is tailored to the location and severity of the fistula. Ongoing advances in minimally invasive techniques are improving safety and outcomes for patients with these complex vascular conditions.
Stroke in Children
Although often thought of as an adult condition, stroke can also occur in infants and children. Pediatric stroke happens when blood flow to part of the brain is interrupted (ischemic stroke) or when a blood vessel ruptures and bleeds into the brain (hemorrhagic stroke). Causes in children differ from adults and may include congenital heart disease, blood disorders, infections, or underlying vascular abnormalities such as AVMs or moyamoya disease. Symptoms can be subtle—weakness on one side, speech difficulties, seizures, or sudden changes in behavior—making early recognition and urgent medical care critical. Research and collaboration are helping to improve diagnosis, treatment, and long-term outcomes for young patients affected by this serious but often under-recognized condition.

How We Work
A Proven Model for Shared Expertise
At BLT, we believe the quality of care shouldn't be limited by geography. Our collaboration model brings together world-class specialists across Boston, London, and Toronto to evaluate complex pediatric neurovascular cases in real time. Whether through scheduled joint reviews or urgent consults, every case reviewed with BLT receives rapid, thoughtful input from multiple disciplines—ensuring faster answers and improving treatment options.

1
Complex/Rare Cases Identified
Clinicians flag challenging or uncommon pediatric neurovascular cases that would benefit from collaborative expertise, ensuring the right cases are brought forward for review.
2
Monthly Joint
Review
A multidisciplinary team of specialists convenes each month to examine these cases in detail, sharing knowledge, insights, and the latest research.


3
Consensus
Recommendation
Through open discussion, the team reaches evidence-based, consensus-driven recommendations, aligning on the best possible path forward for each patient.
4
Implement Patient Care
Agreed-upon recommendations are shared with the referring clinicians to guide treatment, with the aim of improving patient outcomes and quality of life.


About BLT
A Global Network of Pediatric Neurovascular Experts
We’re building a living ecosystem of care. Whether you're a neurosurgeon, pediatric neurologist, researcher, or a patient, you can reach out to our team, ensuring that complex cases receive global attention.
We are happy to review select cases. Please contact us.